Dr. Able Speaks on Physician Burnout
By Dr. Kelsey L. Able
The first time I heard about burnout, I was a senior internal medicine resident and we were required to attend a lecture about resilience/wellness at 7am. I was post-call and had been up all-night caring for ICU patients. From what I remember, we were instructed about the benefits of meditation, yoga and provided with free counseling service information. I could not comprehend when this would fit into my hectic schedule. After the information was presented, we were then required to fill out a survey for the associated quality improvement project. I’m certain my feedback was vicious. I felt that this presentation was the opposite of wellness for the rotation that I was on. It was a bad look. I did not think much more about wellness until much later. I was focused on my path to fellowship.
In my first year after finishing GI fellowship, I went to a conference with a few of my closest residency friends. We are all in different subspecialties following being Internal Medicine residents together at the University of Kansas. One of my former attendings created something completely different- a conference for women physicians focusing on wellness. While there, I had the opportunity to share ideas and learn from those who were at the end of their careers and quite a few physicians that had stepped away from clinical medicine mostly due to burnout.
For the last decade, training programs have been talking about burnout. It’s imperative to appreciate that burnout can lead to anxiety, depression, substance and alcohol abuse, decreased quality of care for patients (errors), and physicians leaving medicine or worse, dying by suicide. I was determined to build better habits, work on efficiency and take a keen interest in my own mental health and wellness. I heard about how therapy should be part of every physician’s armamentarium. I learned about physician coaches. The benefit of coaching has even been published in JAMA in 2019 and 2022 with the benefits of reducing burnout, imposter syndrome and increasing self-compassion. (1, 2) In 2021, Cleveland Clinic saved $133 million in physician retention due to an internal coaching program they implemented. Some of the presenters shared that they were coaching other physicians on efficiency (ie no more charting at home!) It changed my perspective. It was unlike any other conference I had attended before.
“Our inability to say no, our avoidance and our hiding, often lead us to feelings of immense failure, inauthenticity, and burnout.”
– Sasha Shillcutt, MD
Since starting in private practice Gastroenterology, I’ve made a choice to receive much of my continuing medical education (CME) from conferences that focus on wellness and leadership. I’ve chosen to fill my cup first. What I have learned has made me a better doctor, partner and parent. When we care for ourselves, we stay in practice longer and provide the best care possible for our patients. Medicine is a calling, but it’s also a job. We cannot continually sacrifice ourselves and leave nothing for our families and friends. I’ve learned that I cannot continue to pour into cups that don’t pour into mine.
Many of my colleagues know that I strive to be authentic. Depending on when you catch me in the hall on rounds, I will give you the truth about my day. Transparency with regards to the difficulties we encounter while practicing clinical medicine is something that unites us. Spending time with my colleagues in the physician’s lunchroom and listening to the stories of the day, as well as the challenges, can be a bright spot. This is my way of receiving energy as I’m an extroverted introvert. Sometimes this socialization even saves me a few phone calls because we can coordinate care in complex cases. Often, I seek advice from my more senior colleagues and practice partners. Venting to one another is also quite therapeutic.
In the past 5 years, it has become more challenging to get coverage for my patient’s much needed medications. Medicine is now governed by insurance authorizations, protocols and administrators. Our autonomy as clinicians can feel like it is being constantly undermined. I have found myself being less eloquent when I write letters to insurance companies about why my critically ill IBD patients need guideline-directed therapy. I will often tell my rotating KCU medical students (OMS3, 4s) that the moment I stop being a passionate advocate for my patients is the day I should announce my retirement.
While everyone has their own personal keys to success to avoid burnout and focus on their wellness, I’m happy to share mine. Brief explanations will follow.
- Say no.
- Set boundaries.
- Find your work best friends.
- Leave work at work (see #2).
- Know your worth.
- Find your passion in practice.
- Take your vacation days.
What does it mean to say no? I had been told throughout medical education to always say yes to any opportunity. “Build your CV!” When you say no, your yes means more. Many of the committees or boards you serve on don’t add anything financially. If you aren’t in academics, it also will not contribute to tenure. I’ve decided to follow my heart when asked to take on new leadership roles. If my initial reaction is no, I sleep on it and report my decision the following day. If spread too-thin, I’m not as effective as a leader.
Set boundaries with your patients, administrators and colleagues. Technology has made us too available. When you are off duty, make it known and protect that time. I received lots of patient-related texts while I was on vacation this past week from my nurses and physician colleagues. Everyone was so supportive when I responded that I was hiking in the mountains and would get back with them when I was in the office. It can wait.
My endoscopy team is phenomenal. We are a close-knit group (ie work family) and I enjoy spending time with them while taking care of patients. You are allowed to have fun, be professional and take excellent care of patients. Our practice currently spends a lot of time in hospital performing consultations and urgent procedures. I interact with general surgeons, hospitalists and oncologists frequently. Some of the friendships I’ve made are extremely strong and meaningful to me. I never have the “Sunday scaries” because I love the people who I work with, and I love my job.
Don’t chart at home. Please. It’s dysfunctional and is one of the top reasons that physicians burn out. I break my own rule only when I’m coming back after a long vacation. I will log-in the night before to clear my inbox so that I don’t have to get up 2+ hours earlier to get to the office the next day. I trust my partners to address urgent issues when I’m out and will return the favor when they’re on vacation as well.
The path to becoming a practicing physician requires considerable effort, planning and investment put forth. Understand the current market for your practice. Keep up to date regarding reimbursement changes in your field. Appreciate that you are an expert and know your worth. Invest in yourself. Get a therapist and/or a coach. I have a few catch-phrases in clinic but one I’ve said a lot lately is “I have a therapist and you should too.” Brain-gut axis disorders are extremely common.
If you find yourself gravitating towards certain cases, and patient populations, lean into it! Patients appreciate it when we are empathetic and truly invested in their care.
Use your vacation days. Don’t keep rolling them over to the next year. Physicians who took more than three weeks of vacation a year had lower rates of burnout than those who took less. (3). Vacation time is linked to well-being and job satisfaction according to Sinsky, et al.
Don’t pour from an empty cup. Find your pain points in your practice or day-to-day. Focus on what you can control, or delegate. Say no. I’ve been told that “no” is a full sentence by some very brilliant leaders. Leave positions or committees that you aren’t passionate about. Don’t let medicine be your entire persona. Care for yourself the way that you care for your patients. In my opinion, there is no such thing as work-life balance. It will never be balanced. You have the opportunity to choose yourself first. Care for your body and your brain. You matter.
1 Dyrbye LN, Shanafelt TD, Gill PR, Satele DV, West CP. Effect of a Professional Coaching Intervention on the Well-being and Distress of Physicians: A Pilot Randomized Clinical Trial. JAMA Intern Med. 2019;179(10):1406–1414. doi:10.1001/jamainternmed.2019.2425
2 Fainstad T, Mann A, Suresh K, et al. Effect of a Novel Online Group-Coaching Program to Reduce Burnout in Female Resident Physicians: A Randomized Clinical Trial. JAMA Netw Open. 2022;5(5):e2210752. doi:10.1001/jamanetworkopen.2022.10752
3 Sinsky CA, Trockel MT, Dyrbye LN, et al. Vacation Days Taken, Work During Vacation, and Burnout Among US Physicians. JAMA Netw Open. 2024;7(1):e2351635. doi:10.1001/jamanetworkopen.2023.51635
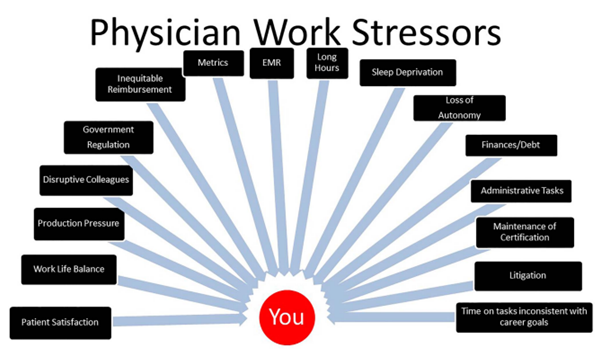
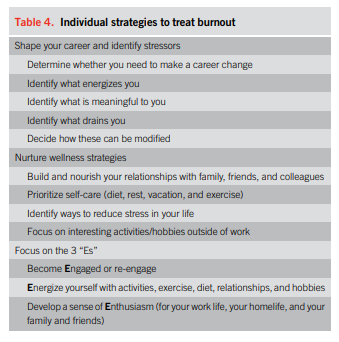
Image 1 and Table 4: Burnout in Gastrointestinal Providers
Lacy, Brian E.; Cangemi, David J.; Burke, Carol A.
The American Journal of Gastroenterology. 119(7):1218-1221, July 2024.
Other resources:
Self Compassion, Kristen Neff PhD
Between Grit and Grace, Sasha K. Shillcutt, MD
Burnout, The secret to unlocking the stress cycle by Emily
and Amelia Nagoski

Dr. Kelsey L. Able
Dr. Able was born in Kansas City, Missouri and was raised in Leawood, Kansas. She attended Kansas State University for undergraduate studies. She then attended Kansas City University for her masters in biomedical sciences and doctorate of osteopathy.
She went to the University of Kansas for internal medicine residency and the University of Oklahoma in Oklahoma City for gastroenterology fellowship. She currently serves as the CIG (consultants in gastroenterology) board president. Dr. Able is honored to serve as the medical ethics committee chair at North Kansas City Hospital. When she isn't scoping and talking to patients about the brain-gut axis, she is spending time attending activities for her two sons, 9 and 6 and enjoying her husband's cooking.